Introduction: Essential nutrients such as iron and B12 have been established as vital components required for hematopoiesis. Patients are at risk of significant comorbidity when these are deficient, including hematologic manifestations and neurological deficits. B12 supplementation is relatively easy to use with no direct adverse effects. Current guidelines use a singular serum cobalamin level < 150 pmol that is static in nature and not adjusted based on patients' underlying age, comorbidities or medications. Many studies have shown symptoms related to deficiency can appear prior to reaching current biochemical definition of deficiency . Methylmalonic acid can be used to detect B12 deficiency earlier, with a sensitivity of approximately 95% however it's utility is limited due to lack of confidence in interpreting it's results and lack of availability . Also, little guidance is provided to clinicians in choosing a method and duration of supplementation in guidelines.
Objective : The primary objective of this study was to establish an expert based consensus recommendations for the diagnosis of B12 deficiency using different biochemical tests while accounting for various comorbidities in diverse patient populations. The secondary objective was to provide recommendations around appropriate and cost-effective B12 supplementation when indicated.
Methods : A detailed literature review was used to generate evidence based statements around diagnostic thresholds for B12 deficiency in various populations as well as guidelines to determine current target doses. A modified Delphi approach was used to evaluate the statements amongst 28 experts in various specialities, including biochemistry, general internal medicine, hematology, nephrology, gastroenterology, geriatrics, obstetrics/gynaecology and paediatrics. Two online survey cycles were performed. Only statements reaching consensus (score >7 by more than 70 % of the experts and a Cronbach's alpha statistic > 0.80) were included in the final iteration . Statements with a score of 5 or greater by <50% of the total respondents were discarded. Statements that were in between these ranges were adjusted based on comments and these new statements were disseminated for round two.
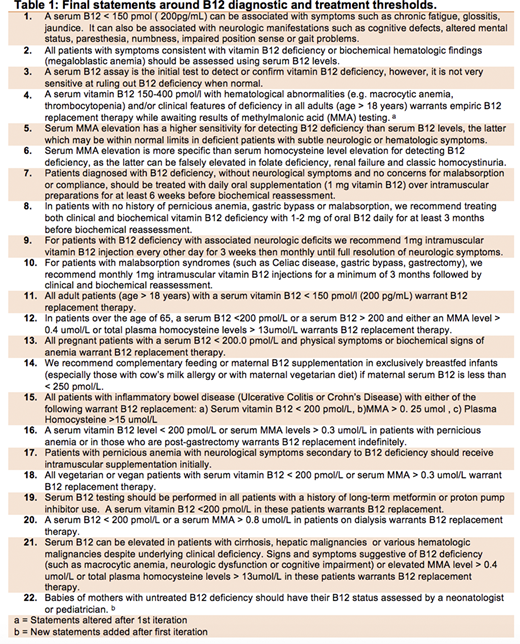
Results: After the first cycle consensus was reached for 20 out of 21 of the statements (Table 1). Based on feedback 1 statement was split and one new statement was added. Only one statement, which was around the use of methylmalonic acid as an adjunct to diagnose B12 deficiency, did not meet consensus after the second cycle. A total of 22 statements achieved the pre-determined cut-off for consensus at the end of round two. An opt out rate of 28- 72 % was observed in statements made regarding the obstetric and paediatrics' population compared to less than 25 percent in all other statements.
Discussion: This guideline provides a summary of B12 diagnostic and treatment threshold for various population that is both supported by existing literature and expert opinion. The high rate of consensus in our first round appears to be due to comfort around prescribing and overall safety of B12 supplementation. Statements made around methods of supplementation and duration were widely accepted. Most clinicians agreed that oral replacement was sufficient for patients unless there was evidence of neurological symptoms or previous gastric surgery . This is important given recent literature indicating the high cost Ontario faces due to inappropriate intramuscular B12 prescribing . A high opt out rate was noted in statements predominately geared towards the paediatric and obstetrical patient population which may be due to discomfort around prescribing in specific populations by general clinicians. Using a modified Delphi methodology, we were able to obtain consensus around adjusted diagnostics thresholds for identifying B12 deficiency in patients with varying comorbidities and metabolic demands. We devised guidance around treatment modalities and timelines to decrease the risk of supplementations faced by patients and potentially the health care system. We hope that these statements can be used as a framework for clinicians in all specialities to provide individualized, evidence based care.
Sholzberg:Amgen: Honoraria, Other: Scientific Advisory Board, Research Funding; Octapharma: Honoraria, Other: Scientific Advisory Board, Research Funding; Novartis: Honoraria, Other: Scientific Advisory Board; Takeda: Honoraria, Other: Scientific Advisory Board, Research Funding; NovoNordisk: Honoraria, Other: Scientific Advisory Board.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal